Cervical cancer is preventable. Get screened.
[4 MIN READ]
In this article:
-
Cervical cancer is one of the most preventable cancers, but it claims the lives of about 4,000 people a year.
-
Cervical cancer is caused by the human papilloma virus, which will likely affect nearly everyone who’s sexually active at some point. Most infections go away on their own, but those that linger can lead to cancer.
-
A Providence Swedish gynecological oncologist outlines the latest screening guidelines and explains why early detection is so important.
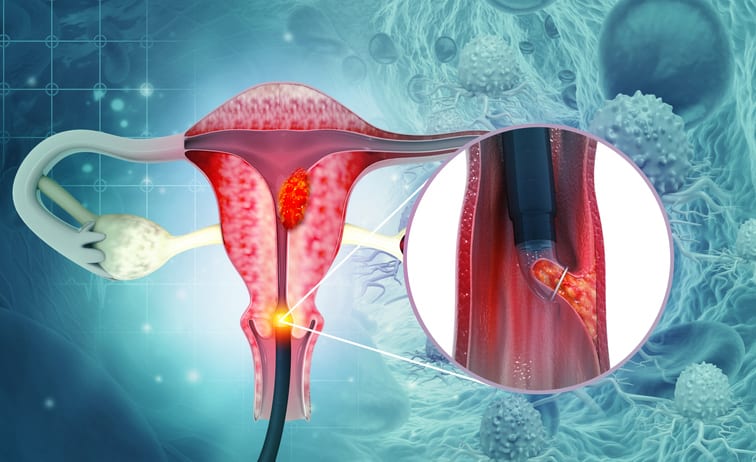
Screening and vaccination have made cervical cancer one of the most preventable forms of cancer, and yet, research indicates the number of people diagnosed with late-stage cervical cancer is increasing. In fact, more than 13,000 new cases of cervical cancer are diagnosed every year, and roughly 4,000 people die from the disease, according to the American Cancer Society (ACS). And some of those deaths could have been prevented.
Cervical cancer is caused by the human papilloma virus (HPV). Nearly everyone who’s sexually active will become infected with HPV at some point. However, most HPV infections go away on their own once your immune system kicks in and gets the infection under control. When the infection lingers, it can cause changes in cervical cells that could develop into cervical cancer.
Joshua Z. Press, M.D., a gynecologic oncologist and cervical cancer expert at Swedish. He took time recently to speak with us about the growing number of cases in the United States, recent changes to screening guidelines and how to prevent cervical cancer.
Vaccinate early, screen regularly
Protecting yourself against cervical cancer is relatively straightforward, according to Dr. Press. “Nothing beats vaccination, screening and early detection,” he explains. “Screening is the most important step. Most patients that I see who come in with cervical cancer have not done their screening, and that’s disappointing. For the screening guidelines to work, you have to follow them.”
Screening guidelines
The ACS updated its cervical cancer screening guidelines in 2025. Changes to the recommendations included raising the age from 21 to 25 to start screening and using an HPV test as a primary screening tool.
There are two main types of cervical cancer screening:
- The HPV test looks for the presence of the human papillomavirus.
- The Pap test looks for precancers, or cell changes on the cervix, that have the potential to become cancer if left untreated.
ACS ecommendations now state:
- Screenings should begin at age 25.
- An HPV test collected by a physician or clinician every five years is the recommended screening method.
- An alternative screenening method of a self-collected HPV test every three years
- People older than 65 do not need a cervical cancer screening if their prior two test results were normal.
“Cervical cancer is one type of cancer that has good, effective screening,” says Dr. Press. “Even if you’ve been vaccinated against HPV, you should still get screened.”
HPV vaccine
The HPV vaccine is a safe, effective way to prevent cervical cancer. The vaccine offers the most protection when given to someone who’s not yet sexually active, and therefore has not been exposed to HPV. It may be given starting at age 9. It is administered in a series of either two or three doses, depending on your age.
Recommendations from the U.S. Centers for Disease Control and Prevention are:
- Starting at age 11 or 12 should get two doses of HPV vaccine, given six to 12 months apart.
- Children who start the HPV vaccine series on or after they turn 15 need three doses of HPV vaccine, given over a six-month period.
- Everyone through age 26 should get an HPV vaccine if they were not vaccinated when they were younger.
- Some adults aged 27 through 45 who have not been vaccinated might choose to get an HPV vaccine after speaking with their doctor.
Advances in treatment
Some 200,000 women in the United States require treatment for cervical cancer every year, says Dr. Press. Fortunately, treatment options for patients with cervical cancer have improved significantly over the past several years.
“For appropriate early-stage disease, we have been able to reduce how aggressive we are with surgery. We can perform a less morbid ‘simple’ type of hysterectomy instead of a radical hysterectomy, which has more risk of complications,” he explains.
“We have also implemented a more precise method to evaluate for spread of cancer cells outside the cervix, called sentinel lymph node dissection. Instead of taking out a large number of randomly selected lymph nodes, we use a fluorescent marker to pinpoint the lymph nodes that actually originate from cervical lymph channels. This marker directs us to the one or two lymph nodes that drain from the cervix, and thus are at risk of containing metastatic cancer cells,” adds Dr. Press.
According to Dr. Press, these new techniques reduce the risks associated with surgery, and allow for quicker post-operative recovery. However, to benefit from these less aggressive surgical techniques, the cancers must be detected in early stage, which highlights the importance of screening and early detection.
Pairing traditional chemotherapy with newer targeted therapies has improved the results for people with more advanced, later-stage cervical cancers. Drugs called angiogenesis blockers inhibit the formation of new blood vessels which prevents tumors from forming or growing larger. Immunotherapy works with your body’s immune system to boost its ability to detect and destroy cancer cells.
“Some of the best responses we’ve seen in advanced cervical cancer are from a combination of traditional chemotherapy combined with both targeted angiogenesis inhibitors and immunotherapy,” says Dr. Press. “With that combination, we’ve been able to get some patients with metastatic disease into remission in a way that we just didn't have in the past.”
There are also new research on a class of drugs called antibody-drug conjugates (ADCs), which has shown promise in developing these treatments chemotherapy-resistant cervical cancer. Learn more about these clinical trials at the Providence Swedish Cancer Institute.
Learn more and find a physican or Advanced Practice Clinician (APC)
If you or a loved one want to learn more about cervical cancer or treatment, the experts at the Providence Swedish Cancer Institute are here for you. To learn more, visit our website, or to speak with someone or make an appointment, call 1-855-XCANCER.
Whether you require an in-person visit or want to consult a doctor virtually, you have options. Contact Swedish Primary Care to schedule an appointment with a primary care provider. You can also connect virtually with your provider to review your symptoms, provide instruction and follow up as needed. And with Swedish ExpressCare Virtual you can receive treatment in minutes for common conditions such as colds, flu, urinary tract infections and more. You can use our provider directory to find a specialist or primary care physician near you.
Information for patients and visitors
Related resources
You can protect yourself from cervical cancer – here’s how
Anyone with a cervix can get cervical cancer
HPV vaccine and regular screenings can reduce cervical cancer risk
This information is not intended as a substitute for professional medical care. Always follow your health care professional’s instructions.
Follow us on Facebook, Instagram and X.
The Providence app offers world-class health care with human connection